
Junior doctors across England have undertaken three days of strike action from 13 to 15 March, during one of the busiest periods of the year for hospitals. This has been a long time coming, with years of stagnant wages and deteriorating working conditions forcing many to consider leaving the country or profession altogether. Six years of university fails to prepare you for the reality of working in the NHS, and I certainly wasn’t cut out for working in clinical medicine. I’m thankful that I found my niche in histopathology where I could continue to practice medicine but in a more controlled and differently, rather than necessarily less, pressured environment.
But I digress. I cannot imagine starting medicine again and working clinically in the current system. Years of systematic underfunding have left the NHS on its knees. Each year the Winter Crisis period gets longer and longer, and soon there will be no summer reprieve. Waiting times will not shorten without significant investment, and while the government pays lip service to improvements, these are rarely seen.

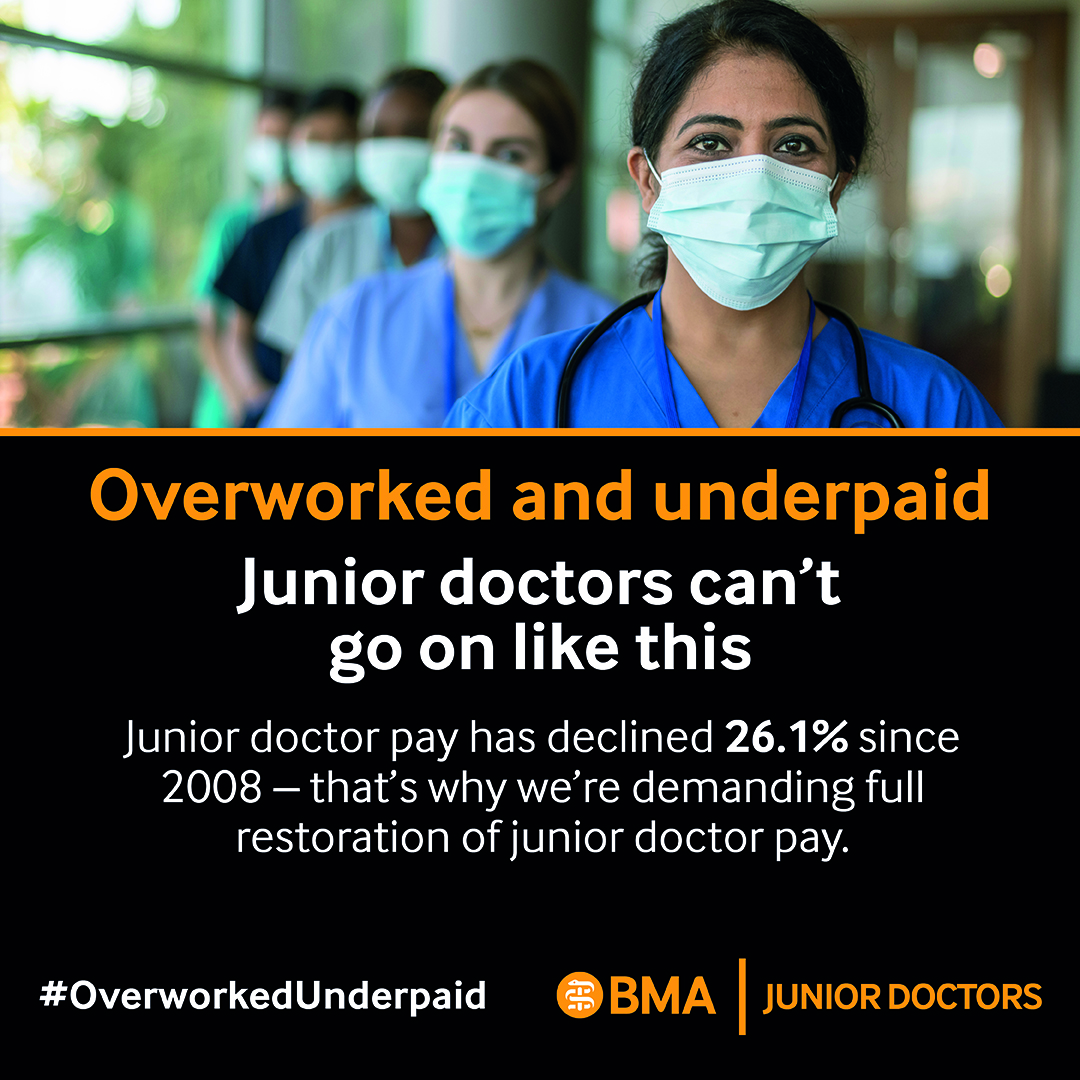
The strikes of 2016 were unsuccessful, but at least part of that was diluted messaging and a complex complaint. This time it’s simple: doctors want pay restoration in line with what we should be paid given inflation, rising cost of living, spiralling tuition fee costs, and a workforce on the brink of giving up. Unfortunately the only bargaining chip we have is strike action, and we do not use it lightly, but to blame all of the problems on these three days of industrial action rather than the thirteen years of Tory government is complete nonsense. Do not believe the media spin.
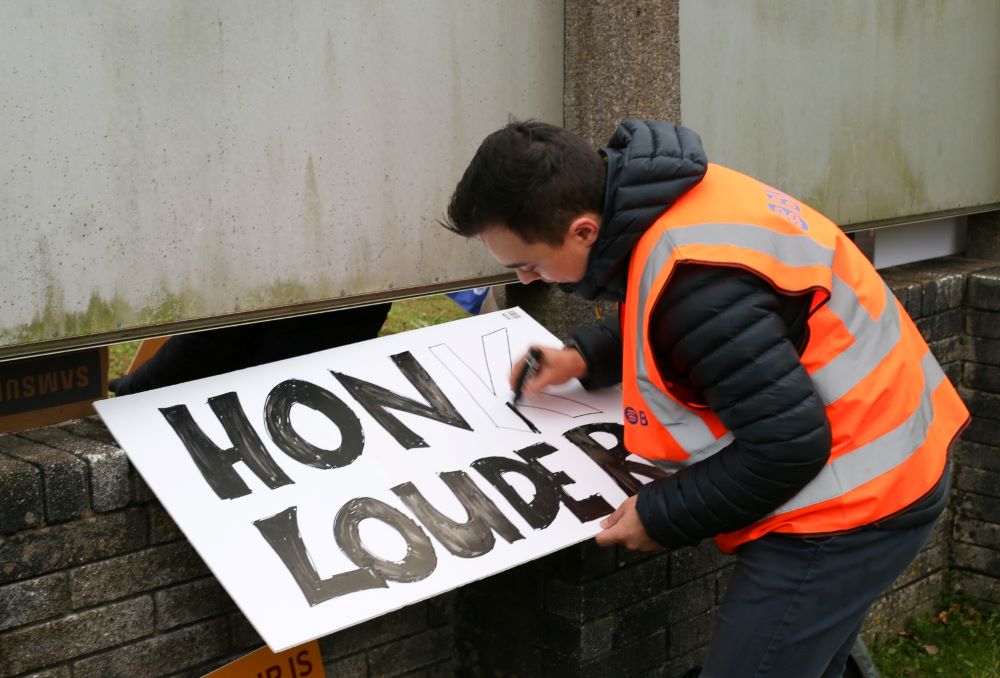
So that’s why I will stand on the picket and support my colleagues. I know that they are an incredibly hardworking, dedicated bunch who have spent years studying in university, working through foundation and core training, progressed through specialist training and spent thousands on exam fees and professional body fees so they could do the job they love. What should be an amazing career is often leaving people burnt out and demoralised, but recognition from the government alongside pay restoration would go some way towards helping keep people in the profession.
Please stand up for your public sector workers so they can be there to help you when you need them most. If you don’t stand up for them, who will?
I’m going to hand the blog over to Sarah for a bit more in-depth explanation of why junior doctors are striking. You might remember her sensational post working as a junior doctor in Northern Ireland in 2016 when colleagues in England were on strike.
So why are Junior Doctors striking?
Let’s take a look at that term “Junior Doctor” for a minute. Many people hear the word “junior” and assume the person they’re going to see will be some fresh-faced student in their late teens or early 20’s. But the reality is that Junior Doctors range from the 23 year old F1 doctor who graduated last month, to the late 30’s or even 40’s ST8 who has spent the last 10 years working as a fully fledged doctor and effectively runs their ward (with the help of our wonderful nursing colleagues and allied healthcare professionals of course). Anyone who is not a Consultant or equivalent is termed a Junior Doctor in the NHS, but that does not make us students or unqualified or whatever else you might have heard.
How does one get to that end goal of Consultant? There are as many paths to becoming a doctor as there are doctors, but for many it starts at school, working your butt off to get those A level grades to claim your place at university. Places on medicine courses are vastly oversubscribed, so this is no easy feat and usually involves taking additional aptitude tests such as the University Clinical Aptitude Test (UCAT) or BioMedical Admissions Test (BMAT). Once you’re there, you spend the next 5-6 years of your life wondering why you didn’t do a course like your housemates with a chance of sleeping in once in a while, all the while accumulating, on average, £43000 of student debt (based on a 2019 average, with costs rising all the time). Many will owe more than this, and I count myself lucky that I entered university before the fee hike and the ridiculous Plan 2 Student Finance repayment plan. If you aren’t au fait with the current repayment plans, just know the interest being charged on Plan 2 loans means doctors in their first few years of post-graduate work are accumulating more in interest than they’re paying off each year.
Once you’ve run the gauntlet of medical school you now have to apply to Foundation Training which lasts for 2 years. At this point, you rank your preferred areas of the UK to work in and hope you did well enough in your exams over the last 5-6 years to get a post somewhere you want to live, with jobs in specialties you want to do. I was lucky in some respects – I got my first choice Deanery, so I didn’t have to move house, but I got my 142nd choice of jobs within that Deanery. In retrospect, it was actually the perfect combination of specialities for me, and even with that I experienced burnout. Many F1 and F2 doctors aren’t so lucky and have to move great distances, sometimes far from family for their first two years of work. After all that, sometime around November in your F2 year you have to decide what you want to do next. Continue in a training program for medicine, surgery, or something else? Take another year to locum and decide what you want to do (known informally as an F3 year)? Leave the UK for sunnier climes? Or maybe leave medicine altogether? I know people who have taken each of these paths for different reasons.
For those of us who chose to enter a training program, this entails another round of applications, interviews and job rankings. If you’re lucky enough to get into a training program, which is by no means guaranteed, you may well have to move to the other end of the country once more. And medicine does not make moving house easy.
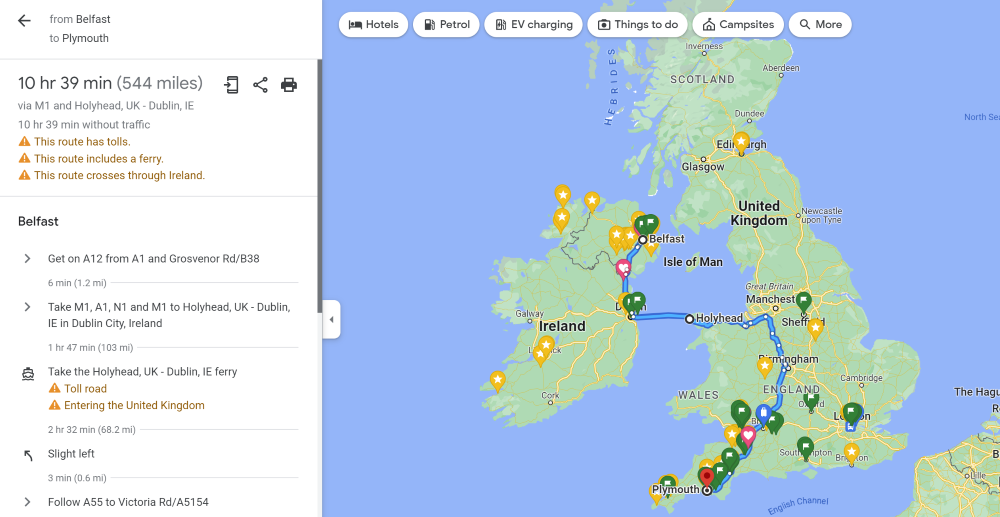
For my part, my F2 job in Belfast ended on the Tuesday and my job in Plymouth (an over 500 mile drive according to Google maps) started the following day. For anyone finishing a job on a night shift, this might mean one job ends at 8am Wednesday morning, while Induction at their new job 500 miles away also started at 8am that Wednesday. It’s a bit of a silly system which requires people to either somehow get annual leave approved for the day before changeover, or to miss Induction at their new Trust and find time to do this at a later date.
Once you start your training program, you then must rotate jobs every 6-12 months. My Deanery has 88 miles between the furthest hospitals we have to rotate through, which means either long commutes, or moving house every year. We can claim travel and relocation expenses back to some degree, but it never quite matches the actual costs involved and takes many months to be repaid. Once again, I will point out that while we are known as Trainees during these 5+ years, we are not students. Yes, we are still learning, but I would argue that in medicine if you’re not still learning every year of your career you’re doing it wrong. The idea that we are students is not helped by the many continuing exams we must do. You would assume that by your mid-30’s you’d have left your days of late night revision and cramming behind, but alas, that is not the case for us. And all of these things must be paid for.
Histopathology (my medical speciality) requires two exams in order to complete training and become a Consultant, although when I started there was another exam, so I have done three. Currently the two exams combined cost £2100, plus an additional £707 if you want to do the additional module available to us. We cannot claim any of this back as study expenses, and a lot of exams happen either in London, or scattered across the country, so we must pay travel and accommodation on top of this. And all this assumes that you will pass your exams first time. In my speciality the part 1 examination has a good pass rate, so most will sit this exam once. Part 2 has a 50% pass rate on average, which means a good proportion of candidates will spend another £1400 on at least one resit attempt. Most other specialties will have similar exam fees.
Add to all this the cost of registration with the GMC (£420 a year), fees to complete training (CCT £452 from the GMC), medical indemnity fees (several hundred pounds, depending on your specialty) and any training courses you wish to attend, which may or may not be funded, and it soon racks up quite a bill just to BE a doctor in the UK. A doctor working full time, i.e. 40 hours a week, will earn £14/hour as an F1 up to £28/hour as an ST6-8. Almost all full-time doctors will work more hours than this, up to a maximum of 48 hours a week, averaged over the length of your rota, and so receive a small boost in pay for this. But not all doctors. Those working in the community, in GP or in some of the Pathology services do not work night shifts or weekends, so they get the basic pay.
The financial burden is huge, but so is the emotional cost. The pressures faced by those working on the wards everyday are innumerable and would take far too much time to list here, but suffice to say, they deal with people at their very best and their very worst, which can involve verbal and physical abuse. Even when patients and families are lovely, healthcare workers still see things many of us will be lucky to never have to experience.

If you want an NHS that is free at the point of care and available to everyone in their time of need, it must be funded properly. There must be the facilities available for healthcare workers to deliver care to the standard they wish they could. There must be proper funding of the diagnostic services the public don’t see, but which are so vital to the running of the NHS. There must be proper remuneration for all staff involved in the running of the NHS, from porters and nursing assistants, to doctors and nurses. Because if you don’t pay people properly, they’ll leave.
Without its staff, what is the NHS?
You can follow Adam on his blog.




