“And my Lord Mayor commands people to be inside by nine at night that the sick may leave their domestic prison for air and exercise”.
Samuel Pepys’s diary 12th August 1665
Throughout recorded history plagues and pandemics have had the capacity to cause massive loss of life. Those in power have sought to control or prevent epidemics, often with little or no scientific basis. As a retired medical microbiologist I’ve looked back at some historical interactions between science, public health and government.
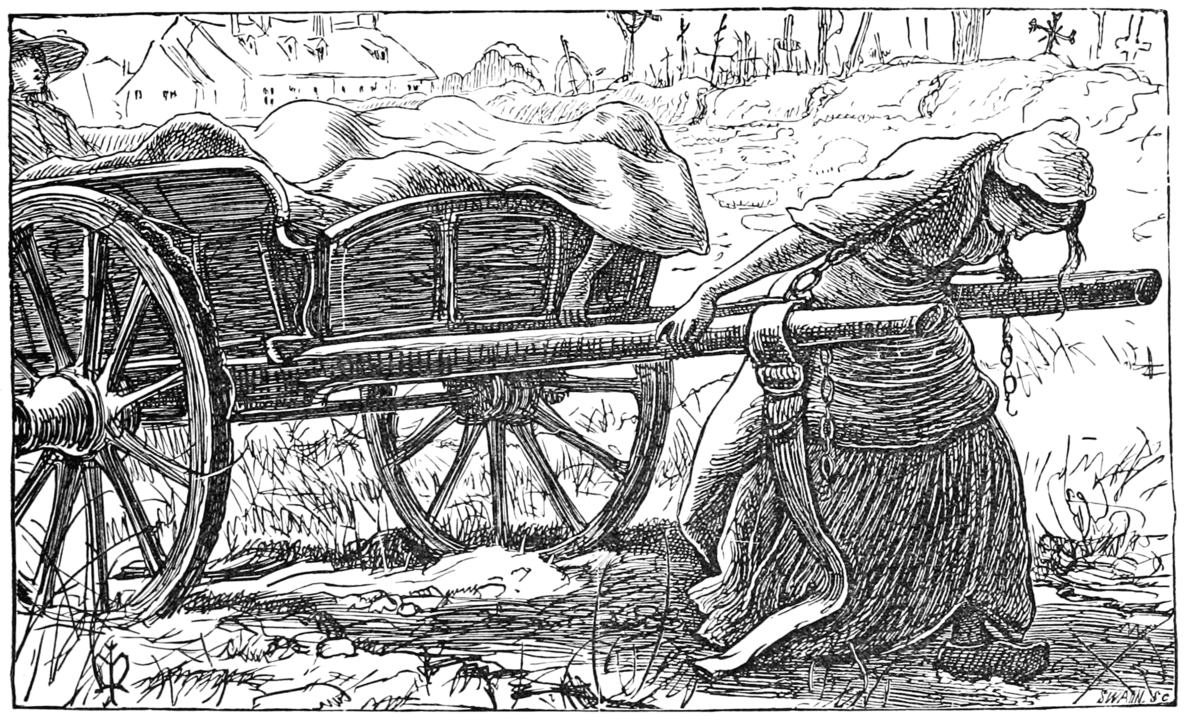
The birth of public health: driven by economic motives
The first proactive step on the road to improving public health was actually driven by an economic argument. Edwin Chadwick (architect of the 1834 Poor Law) believed that decreasing the huge burden of acute infectious disease in male breadwinners would result in reduced demand for poor relief. This required provision of sewers and clean drinking water implemented by new Local Health Boards. Despite argument and delay, after a severe epidemic of cholera, the Public Health Act was finally passed in 1848.
The impact of subsequent improvements in sanitation and water quality was dramatic, with the incidence of diseases such as cholera and typhoid plummeting. In the twentieth century, scientific advances allowed government to implement immunisation programmes which led to dramatic declines of a plethora of infectious diseases.
When fighting Germany was more important than fighting a pandemic
The greatest pandemic of modern times hit the world in three waves between 1918 and 1919 and killed at least 50 million people. Incredibly, it wasn’t discussed by the British Cabinet, even after Prime Minister Lloyd George was affected. The nature of viruses was unclear, so science had little to offer. During a Commons debate on the pandemic, Conservative MP Claude Lowther asked: “Is it a fact that a sure preventative against influenza is cocoa taken three times a day?”
After the first wave, the Chief Medical Officer of the Local Government Board Sir Arthur Newsholme drew up a strategy for responding to a second wave including self-isolation and social distancing. However, in August 1918 he decided that maintaining the war effort was more important,and didn’t issue the advice.
The typhoid outbreak that could have been prevented
Between 1896 and 1946 the incidence of typhoid in the UK fell from 182 to 1 per million. When an outbreak hit Aberdeen in May 1964 with 500 hospital admissions and 19 deaths it caused a media sensation.
Three related but smaller outbreaks had occurred in England between May and October 1963. Science definitively established the source of the first outbreak as corned beef from factory E25 in Argentina, where river water containing sewage was used for cooling cans. Contamination of the contents would have been via tiny defects in the can.
Despite this evidence, no action was taken initially, because both the Ministry of Health and the Ministry of Agriculture Fisheries and Food (MAFF) were anxious to avoid adverse publicity. For MAFF this related to delicate negotiations with the Argentine government about limiting beef exports to the UK.
When another factory (1A) was found to be using untreated water, several consignments of 1A corned beef in transit were stopped, but cans already in Britain weren’t recalled, later causing the Aberdeen outbreak. Civil servant secretiveness and conflicting political pressures prevented definitive action which might have avoided the Aberdeen outbreak.
“The worst treatment disaster in the history of the NHS”
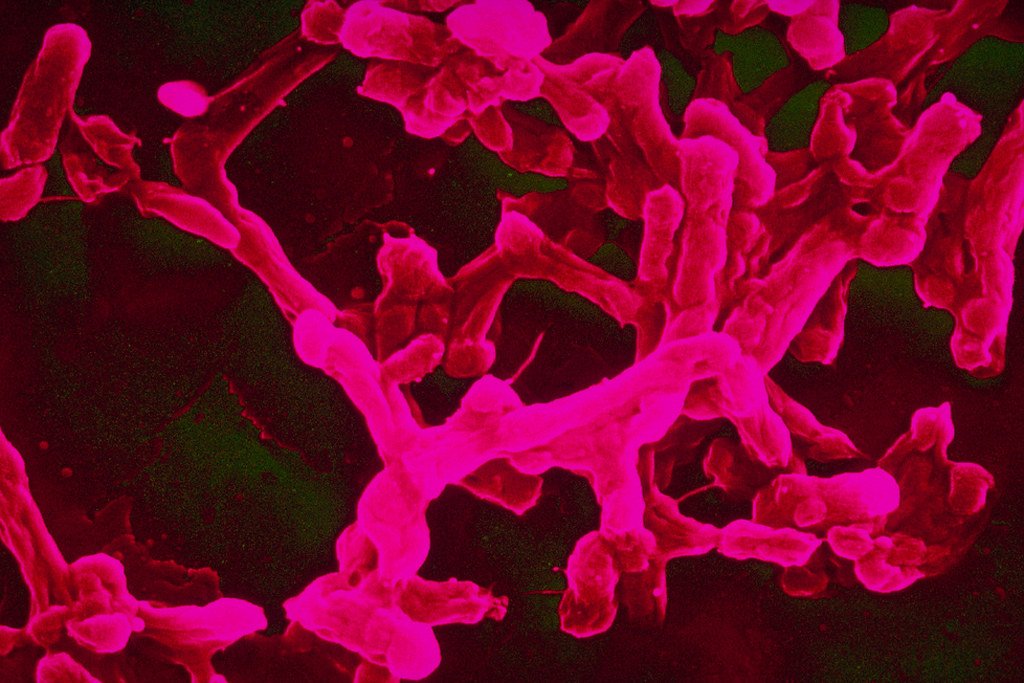
In 2017 The Infected Blood Inquiry started to investigate how, from the 1970s onwards, thousands of patients came to be infected with Hepatitis C and/or HIV from infected blood or blood products.

Worst affected were Haemophilia A sufferers. In the late 1960s a major medical advance allowed bleeds to be treated with concentrated Factor VIII from donated plasma. However the NHS supplier BPL was unable to meet demand. From 1973 hugely expensive but more potent US commercial products were imported. These pooled plasma from tens of thousands of paid donors among whom were prison inmates and drug users who were known to be at much higher risk of transmitting blood-borne viruses such as hepatitis.
The World Health Organisation (WHO) warned about the danger of using these products and in 1974 health minister Dr David Owen made a firm commitment to achieve UK self-sufficiency in blood products, partly on the grounds of reducing costs. Disgracefully it took 13 years to achieve this.
There were numerous contributing factors including:
- The hepatitis (later identified as hepatitis C) was erroneously seen to be mild.
- Doctors and patients liked the convenience and efficacy of the US products.
- BPL was neither managerially nor physically suitable for the scale of mass production required.
- Between 1974 and 1987 there were numerous changes of minister responsible.
- Patients were kept largely in the dark so there was no outcry to drive the process.
Even the advent of HIV didn’t trigger immediate action. Despite evidence to the contrary, in November 1983 the UK health minister Ken Clarke told parliament that “there is no conclusive evidence that AIDS is transmitted by blood products” and the importation of infected products continued.
It took over 40 years to get a public inquiry, by which time those who could be found at fault were either retired or dead. In the interim numerous documents including David Owen’s ministerial papers, committee minutes and hundreds of DHSS files have “disappeared”, further stoking concerns about a cover-up.
Curry’s egg cock-up
Between 1986 and 1988 there was a huge increase in human salmonella cases due to one strain Salmonella enteritidis pt 4. Investigations showed these cases were frequently associated with consumption of eggs.
In August 1988 the Chief Medical Officer issued advice to the public to avoid eating raw eggs and uncooked foods made from them. An angry egg industry challenged the basis for this.
Clearly frustrated, on 3 December 1988 Junior Health Minister Edwina Curry went way beyond the science and told ITN: “Most of the egg production in this country sadly is now infected with salmonella.” Sales of eggs plummeted by 60% overnight. Farmers had to slaughter 4 million hens and destroy 400 million unwanted eggs. MAFF officials were “very angry” at Curry’s remarks and she was forced to resign. The British Egg Industry Council took out adverts in all the newspapers claiming a risk of just 1 in 200 million.
Curry was correct to stress the significance of the issue but wrong to say that most egg production was infected. Large studies later showed that examining boxes of six eggs, around 1% were infected; more than enough to cause the rise in human cases. The furore she created highlighted the issue and probably turbocharged control measures. Ultimately a vaccine was introduced at British lion mark farms causing a dramatic fall of infection in flocks and a huge drop in human cases of S. enteritidis pt 4.
The burger stunt with a tragic outcome
After the sensational emergence of the bovine spongiform encephalitis (BSE) outbreak in cattle in 1986 and the ensuing mass slaughter of infected animals, the Government spent ten years stating that there was no evidence that BSE could be transmitted to humans and that British beef was safe. Infamously, John Gummer in May 1990 tried to persuade us of this by getting his daughter Cordelia to eat a beef burger in front of the media.
On 20 March 1996, Stephen Dorrell, Secretary of State for Health, announced in Parliament that ten young people had contracted a new variant of Creutzfeldt-Jakob disease – vCJD – and that it was probable that they had caught BSE. Further cases of vCJD were to follow (around 178 to date) all of whom have died including Elizabeth Smith, the 23-year-old daughter of a close family friend of Gummer. The link with BSE was subsequently confirmed beyond all doubt. Dorrell’s announcement led to a massive loss of public trust and may have contributed to John Major’s election defeat in 1997.
BSE was difficult: it was a new disease, science couldn’t provide quick answers and there was an underlying conflict of interest between the livelihoods of beef farmers and protecting human health.
Scientists rapidly reached the conclusion (correctly) that BSE was a consequence of recycling of animal protein from rendering plants into ruminant feed. However they mistakenly concluded that BSE had come from the offal of sheep infected with a similar disease scrapie.
In 1988, largely on the basis that scrapie had been around for 200 years without human cases from eating lamb, an expert panel concluded that “it was most unlikely that BSE would have any implications for human health”. This conclusion was not based on hard scientific evidence, merely expert opinion. Nevertheless ministers acted as though it were established fact that eating beef was completely safe.
The subsequent BSE public inquiry reported in 2000 that the government had not lied. However, many issues were identified including:
- Problems with relationships between ministers and officials and between MAFF and Department of Health (DoH).
- The assumption that scrapie was the origin of BSE reduced the urgency to instigate measures to protect human health.
- Several control measures were either impractical, inadequately supervised or delayed in implementation.
- A blanket statement that British beef was safe reflected government concern: to admit that transmission to humans hadn’t been absolutely excluded would destroy the beef industry and cause panic.
Conclusions
The most dramatic improvements in public health in the last 150 years came from improved sanitation, provision of clean water and immunisation programmes, all driven by government. However, in the heat of a major outbreak when government action is crucial, again and again the response seems to be disappointing due to a multiplicity of factors:
- Major outbreaks come along as “banana skins” that can both disrupt a government’s agenda and cause adverse publicity.
- Conflicting priorities and poor communications between ministries, particularly Health and Agriculture, can compromise the appropriate public health response.
- Ministers may not appreciate the basis and rigour of crucial evidence before deciding how to act.
- Science isn’t always tidy; politicians must learn to deal with uncertainty and transparency. It’s an easy get-out to keep quiet in order to “avoid causing unnecessary public alarm”.
- Governments face a public health paradox: prevent illness from occurring and get accused of enacting unpopular and unnecessary measures; or wait to act and then be blamed for avoidable deaths.
- Cabinet reshuffles and changes of government may lead to important actions being delayed or lost.
In the words of Winston Churchill, exemplified by the UK government response to Covid-19: “those who fail to learn from history are condemned to repeat it”. The risk of a further pandemic with a different organism is rising inexorably, so lessons from the past and the Covid-19 pandemic need to be learned and acted on PDQ.
Read this article for more information on the recently-published findings of the all party parliamentary group’s report into the government’s handling of Covid-19.





